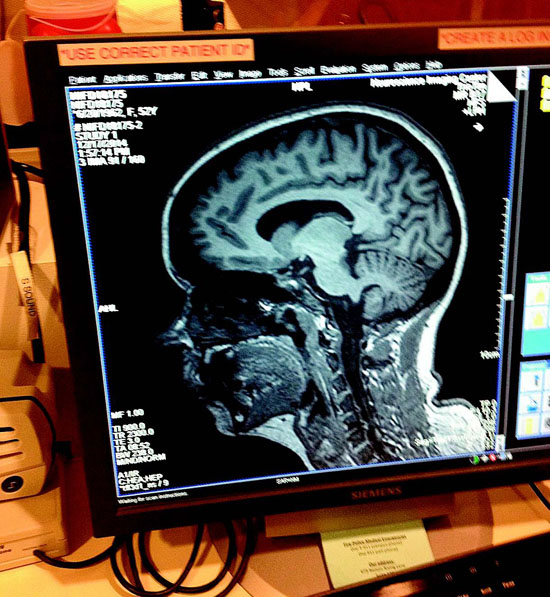
 | | | A view of Ms. Tyson's brain with normal frontotemporal lobes. Image courtesy UCSF | | | | | | Turns out the most difficult part of getting my head examined was not lying still in a snug MRI cave for an hour, but the traffic getting to the impressive facility at UCSF and back. To be fair though, I did decline the less than tempting and possibly painful option of the lumbar puncture that would have topped the difficulty list.
 Looking to participate in some kind of meaningful community service, I happened to see an advertisement in the San Francisco Chronicle seeking volunteers to help out with a brain research study. The initial requirements were easy - being in the right age group of 45 to 55, having no significant deficits in memory or cognition, and perhaps most importantly, not being claustrophobic.
Looking to participate in some kind of meaningful community service, I happened to see an advertisement in the San Francisco Chronicle seeking volunteers to help out with a brain research study. The initial requirements were easy - being in the right age group of 45 to 55, having no significant deficits in memory or cognition, and perhaps most importantly, not being claustrophobic.
 Kind of a mouthful, the Neuroimaging in Frontotemporal Dementia study tracks the progression of a type of dementia that causes the devastating loss of social and cognitive functions as the frontal and temporal lobes of the brain - critical for behavior, emotions and language - atrophy or shrink.
Kind of a mouthful, the Neuroimaging in Frontotemporal Dementia study tracks the progression of a type of dementia that causes the devastating loss of social and cognitive functions as the frontal and temporal lobes of the brain - critical for behavior, emotions and language - atrophy or shrink.
 Frontotemporal dementia is the most common cause of dementia and affects as many people as Alzheimer's disease in those under age 60. Head Researcher Dr. Howard Rosen from the UCSF Department of Neurology is evaluating several different tests to guide diagnosis and treatment of frontotemporal lobe degeneration, or FTLD.
Frontotemporal dementia is the most common cause of dementia and affects as many people as Alzheimer's disease in those under age 60. Head Researcher Dr. Howard Rosen from the UCSF Department of Neurology is evaluating several different tests to guide diagnosis and treatment of frontotemporal lobe degeneration, or FTLD.
 Scientists have made advances in understanding the biological causes of this type of dementia, but at the moment there's no cure and no way to slow its progression. Treatment involves managing the symptoms. As these lobes of the brain gradually shrink, changes in behavior and personality become apparent; those with the disease may become socially inappropriate, impulsive or emotionally indifferent and may lose language skills.
Scientists have made advances in understanding the biological causes of this type of dementia, but at the moment there's no cure and no way to slow its progression. Treatment involves managing the symptoms. As these lobes of the brain gradually shrink, changes in behavior and personality become apparent; those with the disease may become socially inappropriate, impulsive or emotionally indifferent and may lose language skills.
 Developing specific biological measurements or biomarkers are needed to provide precise and direct measurements of the state of the brain which will improve clinical trials for eventual treatments. The real heartbreak of the disease is that it tends to occur at a younger age than does Alzheimer's disease - generally between ages 40-75. The other interesting wrinkle to the disease is that more than half the people have no family history of dementia.
Developing specific biological measurements or biomarkers are needed to provide precise and direct measurements of the state of the brain which will improve clinical trials for eventual treatments. The real heartbreak of the disease is that it tends to occur at a younger age than does Alzheimer's disease - generally between ages 40-75. The other interesting wrinkle to the disease is that more than half the people have no family history of dementia.
 I had a total of three field trips, two to UCSF and one to the Lawrence Berkeley National Laboratory, for a PET (positron emission tomography) scan. At the very new Mission Bay campus of UCSF in their Memory and Aging Center in June and again in December, I gave blood and urine samples, completed extensive cognitive testing that really made me think, had a neurological exam and of course a full hour in their noisy MRI, or magnetic resonance imaging machine. Fitting into the 22-inch-wide opening wasn't a problem. It was basically an opportunity to focus on breathing and listen to music interrupted only by the loud thumping of the machine.
I had a total of three field trips, two to UCSF and one to the Lawrence Berkeley National Laboratory, for a PET (positron emission tomography) scan. At the very new Mission Bay campus of UCSF in their Memory and Aging Center in June and again in December, I gave blood and urine samples, completed extensive cognitive testing that really made me think, had a neurological exam and of course a full hour in their noisy MRI, or magnetic resonance imaging machine. Fitting into the 22-inch-wide opening wasn't a problem. It was basically an opportunity to focus on breathing and listen to music interrupted only by the loud thumping of the machine.
 In Berkeley, there was tight security getting into the lab, but the PET scan was a piece of cake, blissfully quiet. The radioactive tracer injected into my arm that showed brain function didn't cause any problems. The biggest issue of the day was skipping breakfast, taking a pregnancy test - pregnant women definitely not wanted - and making sure I was metal free, with no zippers or jewelry.
In Berkeley, there was tight security getting into the lab, but the PET scan was a piece of cake, blissfully quiet. The radioactive tracer injected into my arm that showed brain function didn't cause any problems. The biggest issue of the day was skipping breakfast, taking a pregnancy test - pregnant women definitely not wanted - and making sure I was metal free, with no zippers or jewelry.
 My brain is one of a total 240 that will be examined at three facilities: UCSF, the Mayo Clinic in Rochester, Minn., and Massachusetts General Hospital in Boston with sponsorship from the National Institutes of Health. Rosen said they are still looking for additional control group members with no apparent memory problems.
My brain is one of a total 240 that will be examined at three facilities: UCSF, the Mayo Clinic in Rochester, Minn., and Massachusetts General Hospital in Boston with sponsorship from the National Institutes of Health. Rosen said they are still looking for additional control group members with no apparent memory problems.
 Having volunteered for a number of worthy causes over the years, getting my brain examined for a research study was actually interesting and clearly way more effective than my lame construction attempts at a Habitat for Humanity site. Those interested in more information can visit memory.ucsf.edu or call Aly Caplan, research coordinator at UCSF's Memory and Aging Center, at (415) 476-0670.
Having volunteered for a number of worthy causes over the years, getting my brain examined for a research study was actually interesting and clearly way more effective than my lame construction attempts at a Habitat for Humanity site. Those interested in more information can visit memory.ucsf.edu or call Aly Caplan, research coordinator at UCSF's Memory and Aging Center, at (415) 476-0670.

|
